The importance of country-level voices in vaccine development
Here in Ghana, we introduced rotavirus vaccine into our national immunization program in April 2012 and our rotavirus vaccine coverage rates are consistently high. Despite this, many of our children still suffer from rotavirus diarrhea, with an estimated 650 children in Ghana dying in 2019 due to rotavirus. Globally, rotavirus causes about one-third of diarrhea-related child deaths and millions of hospitalizations each year. While current live, oral rotavirus vaccines (LORVs) are lifesaving tools that should be used to reduce severe diarrhea worldwide, they are not as effective in places with the highest burden.
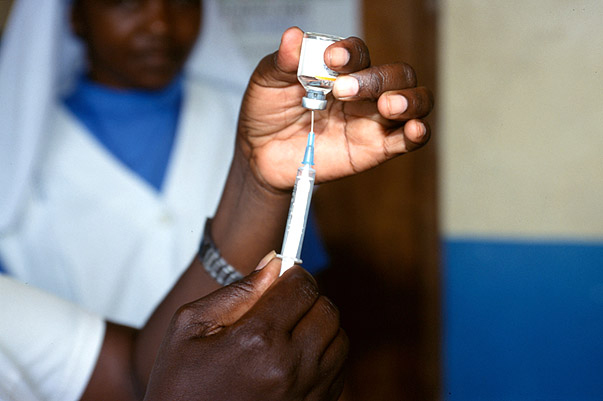
Researchers have been working on several new rotavirus vaccine approaches that may be more effective in places like Ghana and may potentially address barriers to rotavirus vaccine uptake and access. Injectable next-generation rotavirus vaccine (iNGRV) candidates are expected to provide superior efficacy in high-burden settings compared to current LORVs. This is because they bypass the child’s gut, which scientists think is responsible for the lower efficacy seen with oral options. Additionally, because iNGRVs are injected, they could potentially be combined with other injectable vaccines in the childhood immunization schedule, helping to ease delivery efforts and potentially increase uptake.
While iNGRVs sound promising, we recognized an important perspective was missing from this research – the perspective of country-level stakeholders located where rotavirus burden is greatest. Would they want to use an iNGRV? Would it be feasible within their national immunization programs? Local stakeholders are the ultimate decision-makers about introducing new vaccines into their country’s immunization schedule. Yet, vaccine developers generally do not take their perspectives into account when designing candidate vaccines.
Understanding country-level stakeholder perspectives
The childhood immunization schedule is getting more crowded as new vaccines are developed and introduced. It’s important to understand country-level preferences for new vaccines earlier in the development process so that you end up with a vaccine that meets country needs that they can—and want—to incorporate into their vaccination programs.
PATH conducted a series of studies to understand the real public health value of iNGRVs to help inform decisions by international agencies, funders, vaccine manufacturers, and countries. A major component of this work was a feasibility and acceptability study, which entailed interviewing 71 national stakeholders who work in roles that influence vaccine adoption and 64 healthcare providers who administer vaccines in Ghana, Kenya, Malawi, Peru, Senegal, and Sri Lanka to assess their preferences for different hypothetical rotavirus vaccine options.
Across all six countries, study results indicate that vaccine delivery considerations were the most important preference drivers for national stakeholders, followed by improved efficacy and cost. Nearly half preferred a higher efficacy, standalone iNGRV over existing LORVs despite reservations about adding new injections to the vaccination schedule. Most strikingly, a vaccine that combined an iNGRV with a diphtheria-tetanus-pertussis (DTP)-containing vaccine (such as DTP-Hib-hepB) into one formulation was by far the most preferred approach among national stakeholders, even if efficacy was no better than existing LORVs, due to the ease of delivery and lower cost.
Almost all healthcare providers across the study strongly opposed adding a standalone iNGRV to the vaccination schedule due to concerns about adding yet another injection. However, because we wanted healthcare providers to focus on delivery concerns, they were not given efficacy or cost information about the vaccine options, so it’s unclear if assumptions about a higher efficacy or lower cost iNGRV would impact this preference. In contrast, they were quite supportive of using an iNGRV if combined with a DTP-containing vaccine.
As the lead study investigator for Ghana, I interviewed 9 national stakeholders and 10 healthcare providers. Stakeholder preferences in Ghana were similar to the results seen across the other study countries, with a strong reluctance to add new injections to the immunization schedule. However, as Ghana prepares to transition away from Gavi, the Vaccine Alliance co-financing, cost was an essential issue for stakeholders in these interviews and a lower-priced iNGRV was attractive.
What happens next?
These results, combined with findings from other PATH-led studies, help elucidate the circumstances and use cases iNGRVs would offer a compelling public health value proposition. The potential impact, cost-effectiveness, and national stakeholder interest in iNGRVs are markedly dependent on the product profile. While an iNGRV with high clinical efficacy is clearly most desirable, these results also suggest that an iNGRV with efficacy similar to LORVs could be a strongly preferred option if combined with a DTP-containing combination vaccine. These comprehensive findings may help to target donor and vaccine development investments toward the most preferred and cost-effective formulations of iNGRVs, as well as assist in future clinical trial designs and endpoints.
More broadly, feasibility and acceptability studies like this one can help identify which product attributes are prioritized by different stakeholders and why, potentially informing vaccine design and clinical evaluation. In turn, these studies could ultimately facilitate vaccine recommendations and uptake. Gathering input directly from local vaccine decision-makers and healthcare providers must be prioritized for all future attempts to understand the public health value of vaccines, especially those destined primarily for low- and middle-income country markets.
To this end, I’m about to embark on another set of interviews with Ghana stakeholders to gather their preferences about potential Shigella vaccine candidates. Shigella is another leading cause of diarrheal disease and infection and has been linked to long-term health impacts like growth faltering and stunting. While no vaccines against Shigella exist yet, several candidates are in clinical development. To better understand what country stakeholders would want in a Shigella vaccine, especially in the context of many other potentially attractive vaccine and health interventions, PATH is conducting another multi-country stakeholder preferences study as part of a broader public health value proposition.
While it’s important to keep in mind that these new vaccines will be in clinical trials for several more years, I’m proud to be a part of PATH’s work to ensure that country-level voices are being heard and can potentially influence vaccine development efforts.


