The hidden consequences of bacterial diarrhea
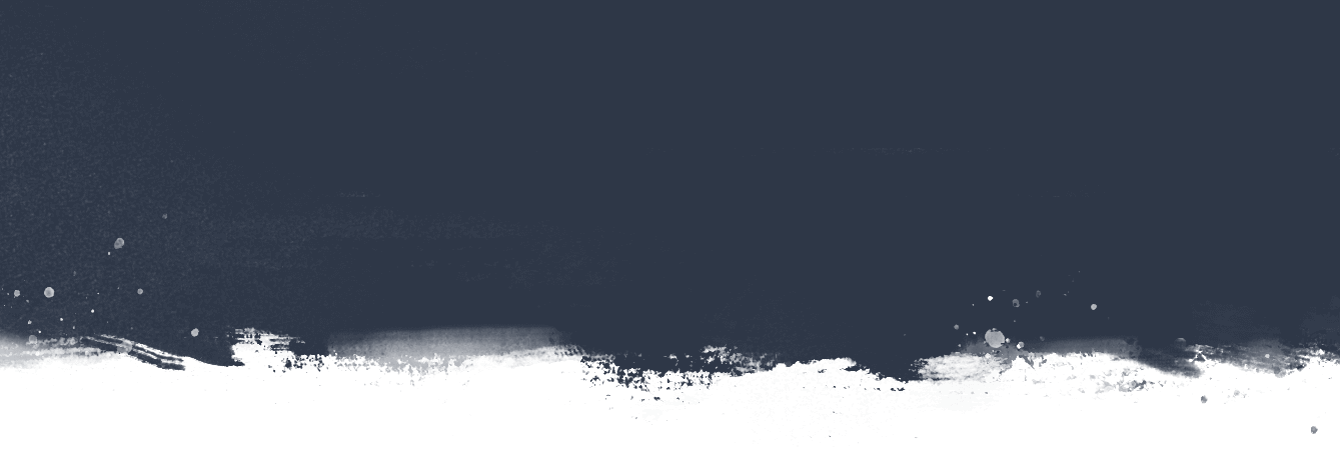
Diarrhea is rarely just diarrhea. While the acute infection can be relatively short-term, lingering long-term consequences like stunting, malnutrition, and financial implications often follow. This is especially true for bacterial diarrhea infections in young children.
ETEC and Shigella: common infections with far-reaching impact
Diarrhea is caused by a wide array of viruses, bacteria, and parasites, but two of the most common pathogens behind repeated infections are the bacteria entertoxigenic E. coli (ETEC) and Shigella. ETEC is often the first enteric pathogen that a baby will encounter in his or her life, and Shigella is the most common cause of severe, bloody diarrhea (dysentery) in young children. Because of the way these bacteria interact with a child’s gut, they can lead to a disorder called environmental enteric dysfunction (EED). Affected children may experience stunted growth and weakened immune systems, which increase the risk of other, sometimes fatal infectious diseases.
ETEC and Shigella are common infections. The sheer number of children affected by both their acute and indirect consequences is part of what makes their impact so far-reaching. That is why scientists and global health stakeholders like the World Health Organization have prioritized these pathogens for vaccine development, and several candidates are in clinical trials. For instance, one ETEC vaccine candidate recently showed promising results in a descending-age trial in Bangladesh, and one of several Shigella vaccine candidates is embarking on a Phase 2 field study. As we continue to develop these vaccines, improved estimates of the wider health burden of these bacteria could help determine the potential impact and cost-effectiveness of various vaccination strategies to guide decision-making.
Estimating the total burden of disease and potential for vaccines
Over the past few years, PATH worked with a team to do just that—attempt to quantify the total ETEC and Shigella disease burden and projected vaccine impact and cost-effectiveness. First, we estimated the morbidity, mortality, and stunting cases associated with ETEC and Shigella infections among 79 low-income and lower-middle income countries. Published in The Lancet Global Health, the results estimated that 196 million episodes of ETEC and Shigella diarrhea occurred among children under 5 in 2015, resulting in 44,400 total ETEC deaths, 63,100 total Shigella deaths, and 3.5 million cases of moderate-to-severe stunting. When we accounted for additional infectious disease mortality due to stunting—i.e., deaths from other infectious diseases that an initial ETEC or Shigella infection predisposed a child to—it resulted in a 24% and 28% increase in estimated mortality due to ETEC and Shigella infections, respectively, compared to direct deaths only. The distribution of mortality and morbidity varied geographically, with countries in the African and Eastern Mediterranean regions bearing the greatest burden.
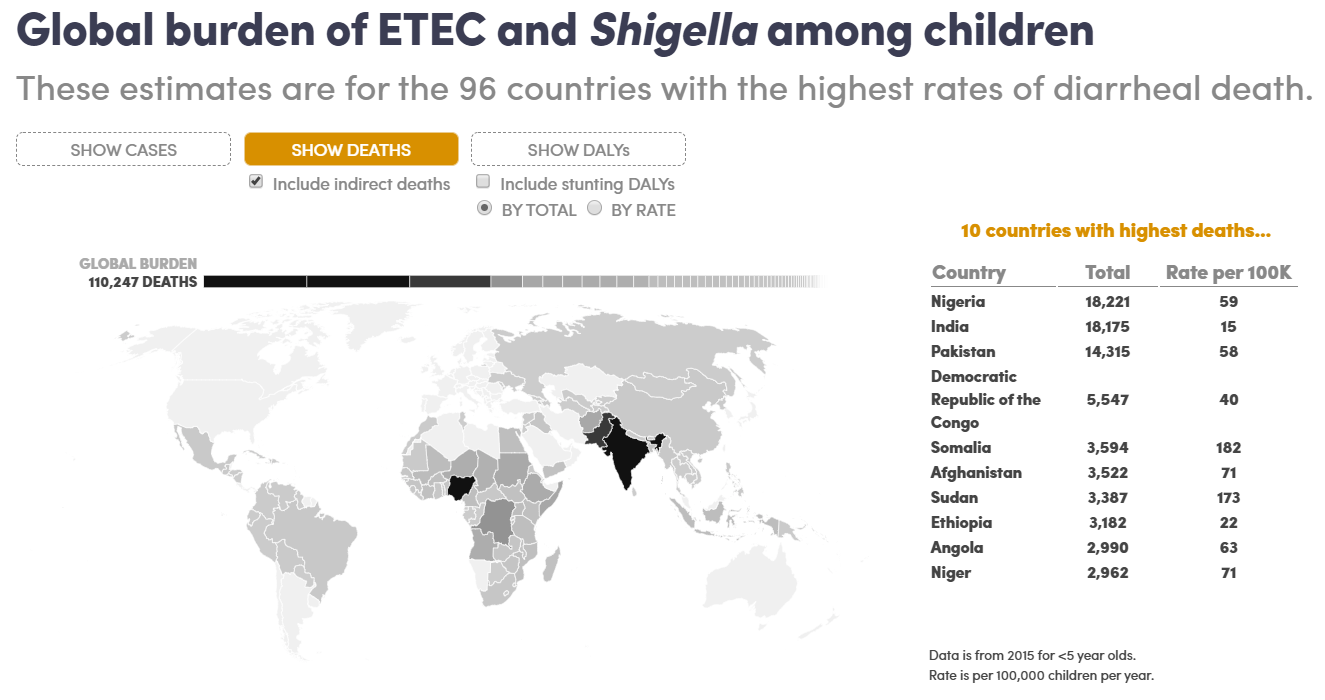 Explore the results of the estimated global ETEC and Shigella burden analysis in more detail in an interactive feature from DefeatDD. Next, the team looked at the projected impact and cost-effectiveness of the vaccines. Published in Vaccine: X, our analysis estimated that, in the absence of vaccination, ETEC and Shigella would cause 239,300 and 340,300 respective child deaths between 2025 and 2034, mostly in African countries. Furthermore, ETEC and Shigella cases would result in over 13.7 and 21.4 million stunted children, respectively. Introducing an ETEC and/or Shigella vaccine, each with a projected 60% efficacy, could prevent 92,000 ETEC and/or 126,600 Shigella direct deaths as well as 21,400 ETEC- and/or 34,200 Shigella-induced stunting deaths. Cost-effectiveness of vaccination varied, with the vaccine being more cost-effective in the African and Eastern Mediterranean regions.
Explore the results of the estimated global ETEC and Shigella burden analysis in more detail in an interactive feature from DefeatDD. Next, the team looked at the projected impact and cost-effectiveness of the vaccines. Published in Vaccine: X, our analysis estimated that, in the absence of vaccination, ETEC and Shigella would cause 239,300 and 340,300 respective child deaths between 2025 and 2034, mostly in African countries. Furthermore, ETEC and Shigella cases would result in over 13.7 and 21.4 million stunted children, respectively. Introducing an ETEC and/or Shigella vaccine, each with a projected 60% efficacy, could prevent 92,000 ETEC and/or 126,600 Shigella direct deaths as well as 21,400 ETEC- and/or 34,200 Shigella-induced stunting deaths. Cost-effectiveness of vaccination varied, with the vaccine being more cost-effective in the African and Eastern Mediterranean regions.
Uncovering inequity in national burden
Another important part of the story is that not all children within a country are equally at risk for ETEC and Shigella. Children of marginalized or rural populations within a country may be more at risk for disease than others in the same country due to a lack of access to clean water and sanitation services, health care services, or increased exposure to other infectious diseases. Therefore, it is important to understand not only the burden, but also the potentially different impact and cost-effectiveness of vaccination, at the subnational level.
Our team published two analyses looking at exactly these questions. In the first analysis, published in The Lancet Global Health, we established a method for evaluating the subnational disease burden in 11 sub-Saharan African countries. We found that some of these countries have substantial heterogeneity of burden, with some regions and populations experiencing a higher burden than others. The second analysis, published in Vaccine: X, examined subnational variation in potential impact and cost-effectiveness of ETEC and Shigella vaccines for four of these 11 countries. We found that vaccination was most cost-effective in averting loss of healthy life in lower wealth subpopulations living in the highest-burden provincial areas. In other words, vaccine impact and cost-effectiveness were more favorable when vaccinations reach the most vulnerable children in underserved provinces. Introducing vaccines only in high-burden countries and regions could substantially reduce cost without substantially reducing impact.
The effects of ETEC and Shigella diarrhea can have lasting consequences. Prevention of these infections through vaccination could reduce the risk of direct deaths, stunting, and deaths due to other infectious diseases. By understanding the countries, provinces, and populations with the highest disease risk and potential benefit of ETEC and/or Shigella vaccination, we can help ensure interventions will target those in greatest need.


