Breastfeeding is a team sport

Breast milk is probably the closest thing we have to a magic potion. It not only contains the perfect blend of nutrients for babies in the first 6 months of life, but it can also kill pathogens, boost a baby’s immunity, and regulate a baby’s sleep-wake cycles. Even more amazing, breast milk changes on a daily basis—and even throughout the course of a single day—depending on environmental factors, a baby’s age, the time of day, and a baby’s other needs as communicated to the mother through the milk-saliva exchange. It’s also one of the best ways to prevent diarrheal disease in young babies. The more we learn about breast milk, the more amazed I become.
When I became pregnant with my first child in 2019, I was excited to gain firsthand experience with this “potion.” As a global health professional who works on Team DefeatDD, I am an avid advocate of the World Health Organization (WHO) recommendation of exclusive breastfeeding for the first 6 months. In preparation, I took a breastfeeding class, read up on the latest research and recommendations, and bought supplies. I was ready!
So you can imagine my surprise when, for the first week of my son’s life, it turned out that he was drinking not my breast milk, but a stranger’s.
 Miles thought the donor milk was delicious! Especially when his dad fed it to him.When things don’t go according to (birth) plan
Miles thought the donor milk was delicious! Especially when his dad fed it to him.When things don’t go according to (birth) plan
My amazing son Miles was born in January 2020, almost a month before his due date. When Miles came out, he was almost immediately taken to the neonatal intensive care unit (NICU). Because of some labor complications and Miles’ being in the NICU, and because breast milk production requires oxytocin—the “love hormone” produced by being with and holding your baby skin-to-skin—my milk was, initially, absent. But Miles needed to eat, of course, so the NICU nurses asked whether I prefer for him to receive formula or donor breast milk?
For me, it wasn’t even a question. I knew that, even if it not perfectly suited for Miles, a stranger’s milk was the next best option to my own milk.
It was also a full-circle moment for me because human milk banking is something PATH supports and advocates for in low- and middle-income countries. The WHO recommends the safe use of donor milk for vulnerable babies, such as low-birth-weight or premature infants, who cannot be fed their mother’s own milk. I was not alone in having difficulty with breastfeeding a premature infant—between 15 and 40% of infants in NICUs worldwide do not have access to their mothers’ milk. For these babies, access to human milk has long-term benefits and can be lifesaving. In the United States and worldwide, use of donor breast milk is limited, but improving.
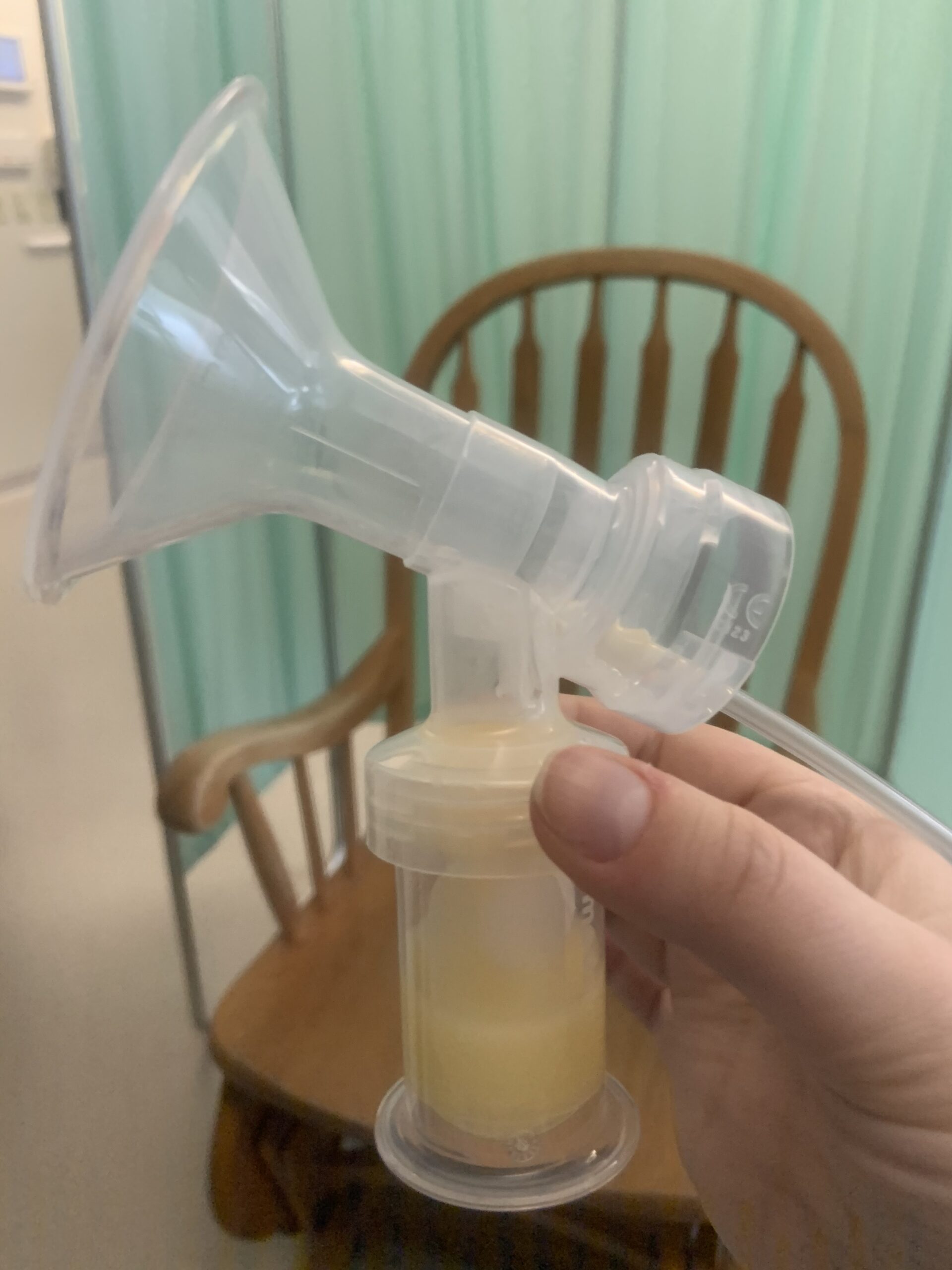 Small amounts of pumped colostrum (the nutrient-rich early breast milk) were a huge win in those early NICU days.Over the course of the next week in the NICU, Miles drank donor breast milk and grew stronger while lactation consultants helped me build my milk supply through pumping. Finally, on the day Miles came home from the NICU, the milk began flowing. We had a few additional difficulties, like needing a tongue tie procedure that further delayed a proper latch. But eventually, nearly a month after he was born, my son latched on and successfully breastfed. I was so happy I cried.
Small amounts of pumped colostrum (the nutrient-rich early breast milk) were a huge win in those early NICU days.Over the course of the next week in the NICU, Miles drank donor breast milk and grew stronger while lactation consultants helped me build my milk supply through pumping. Finally, on the day Miles came home from the NICU, the milk began flowing. We had a few additional difficulties, like needing a tongue tie procedure that further delayed a proper latch. But eventually, nearly a month after he was born, my son latched on and successfully breastfed. I was so happy I cried.
Breastfeeding takes a village
Today, Miles is a healthy and hefty nearly-6-month-old—almost old enough to start trying solid foods!—and we are both pros at breastfeeding. But while our breastfeeding journey had a happy ending after such a difficult start, many mothers are not so lucky. Globally, breastfeeding rates are less than 50%, largely due to a lack of knowledge about the benefits of breastfeeding and a lack of support.
Support, I believe, is the key. Even with all the knowledge I had about breastfeeding and everything I did to prepare, I needed a ton of support to make breastfeeding work. From the kind and generous donors whose milk fed my baby when I could not, from the milk bank that sterilized and stored the breast milk, from lactation consultants and doctors and nurses, and from my job and coworkers after I went back to work. And, most importantly, from my incredible husband and other family and friends who stood by me and encouraged me when I wanted to give up. Because I did want to give up at times. If any of those support mechanisms were missing, I very well may have. I may not have had a choice.
Universal breastfeeding, as a crucial part of universal health coverage, could save an estimated 800,000 infants each year by preventing death and stunting from malnutrition. But almost all mothers have some difficulty. For new mothers in the COVID-19 era, it is especially crucial to maintain availability of support—whether from lactation consultants, nurses, or community health workers—and access to human milk banking.
Breastfeeding is a team sport, and not for the faint of heart. Luckily, mothers have some of the strongest hearts. With assistance from family and friends, health workers, public policies that facilitate milk banking, and generous breastfeeding strangers, I believe it should be possible for all babies to receive the magical miracle that is breast milk.
 Miles is now a healthy, smiley little dude!
Miles is now a healthy, smiley little dude!


